Search
Recent comments
- naked.....
6 hours 5 min ago - darkness....
6 hours 28 min ago - 2019 clean up before the storm....
11 hours 48 min ago - to death....
12 hours 27 min ago - noise....
12 hours 34 min ago - loser....
15 hours 14 min ago - relatively....
15 hours 36 min ago - eternally....
15 hours 42 min ago - success....
1 day 2 hours ago - seriously....
1 day 4 hours ago
Democracy Links
Member's Off-site Blogs
addressing the needs of those affected by covid VACCINATION...
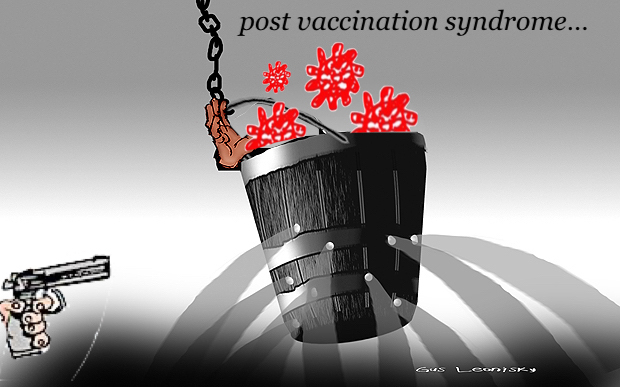
COVID-19 vaccines have been instrumental in reducing the impact of the pandemic, preventing severe illness and death, and they appear to protect against long COVID. However, some individuals have reported chronic symptoms that developed soon after receiving a COVID-19 vaccine. This little-understood, persistent condition, referred to as post-vaccination syndrome (PVS), remains unrecognized by medical authorities, and little is known about its biological underpinnings.
A small number of people report chronic symptoms after receiving COVID-19 shots. A new study provides clues for further research.
In a new study, Yale researchers have taken initial steps to characterize this condition, uncovering potential immunological patterns that differentiate those with PVS from others. The findings are early and require further confirmation but may eventually guide strategies to help affected individuals.
“This work is still in its early stages, and we need to validate these findings,” said Akiko Iwasaki, Sterling Professor of Immunobiology at Yale School of Medicine (YSM) and co-senior author of the study published Feb. 19 as a preprint on MedRxiv. “But this is giving us some hope that there may be something that we can use for diagnosis and treatment of PVS down the road.”
Some of the most common chronic symptoms of PVS include exercise intolerance, excessive fatigue, brain fog, insomnia, and dizziness. They develop shortly after vaccination, within a day or two, can become more severe in the days that follow, and persist over time. More studies are needed to understand the prevalence of PVS.
“It’s clear that some individuals are experiencing significant challenges after vaccination. Our responsibility as scientists and clinicians is to listen to their experiences, rigorously investigate the underlying causes, and seek ways to help,” said Harlan Krumholz, the Harold H. Hines, Jr. Professor of Medicine (Cardiology) at YSM and co-senior author of the study.
Data for the study came from Yale’s Listen to Immune, Symptom, and Treatment Experiences Now (LISTEN) Study, through which researchers aim to better understand long COVID and PVS. For the new study, researchers included data from 42 LISTEN participants who reported symptoms of PVS and 22 individuals who did not report any PVS symptoms after receiving a COVID-19 vaccination.
From participants’ blood samples, the researchers looked for immune features that were different between the two groups. They found several differences in immune cell populations; those with PVS had lower levels of effector CD4+ T cells and higher levels of TNF-alpha+ CD8 T cells — both are types of white blood cells — among other differences.
There were also differences in the levels of antibodies that the body uses to target SARS-CoV-2. Participants with PVS who had never contracted COVID-19 had lower levels of antibodies against the SARS-CoV-2 spike protein than control participants, likely because they tended to have fewer vaccine doses than individuals without PVS. Fewer vaccine doses and no viral infection means the body’s immune system has had little opportunity to develop a defense to the virus, said the researchers.
When the researchers measured levels of SARS-CoV-2 spike protein — the part of the virus that enables it to penetrate and infect host cells and what COVID-19 vaccines use to trigger immune responses against the virus — they found that some individuals with PVS, even those without evidence for infection, had higher levels of spike protein than controls. Typically spike protein can be detected for a few days after vaccination, but some participants with PVS had detectable levels more than 700 days after their last vaccination. Persistent spike protein has been associated with long COVID as well.
“That was surprising, to find spike protein in circulation at such a late time point,” said Iwasaki. “We don’t know if the level of spike protein is causing the chronic symptoms, because there were other participants with PVS who didn’t have any measurable spike protein. But it could be one mechanism underlying this syndrome.”
Krumholz explained that PVS might be similar to how different infections can cause chronic symptoms through distinct biological pathways. “One person might develop chronic symptoms due to immune dysregulation, while another experiences lingering effects from viral reactivation,” he said. “We need to map these different pathways carefully to understand what is happening in each case. This work is just beginning, and further studies are essential to guide diagnosis and treatment.”
Going forward, the researchers want to further validate these findings in a larger group of people “This is far from a final answer on PVS,” said Iwasaki.
They’re also investigating several possible drivers of PVS. Along with spike protein persistence, the researchers are assessing the contributions of autoimmunity, tissue damage, and Epstein-Barr Virus (EBV) reactivation. In the study, individuals with PVS were more likely than those without the syndrome to have evidence of reactivated EBV, which is the most common cause of infectious mononucleosis, also known as “mono.”
A deeper understanding of PVS and its drivers could lead to better vaccines that have fewer side effects, effective methods for diagnosing the syndrome, and targets for treatment, said the researchers.
“For instance, if we can determine why spike protein is persisting for as long as it is in some people, maybe we can remove it — with monoclonal antibodies, for example — and maybe that could help reduce PVS symptoms,” said Iwasaki.
Iwasaki is also a professor of dermatology and of molecular, cellular, and developmental biology in Yale’s Faculty of Arts and Sciences, a professor of epidemiology at Yale School of Public Health, and an investigator of the Howard Hughes Medical Institute.
“We’re only just starting to make headway in understanding PVS,” said Krumholz. “Every medical intervention carries some risk, and it’s important to acknowledge that adverse events can occur with vaccines. Our focus must remain on understanding what these people are experiencing through rigorous science and addressing the needs of those affected with compassion and an open mind.”
YOURDEMOCRACY.NET RECORDS HISTORY AS IT SHOULD BE — NOT AS THE WESTERN MEDIA WRONGLY REPORTS IT.
Gus Leonisky
POLITICAL CARTOONIST SINCE 1951.
- By Gus Leonisky at 24 Feb 2025 - 8:25am
- Gus Leonisky's blog
- Login or register to post comments
health research....
Planned NIH cuts, blocked for now, would imperil vital Yale health research
Yale supported legal efforts that prompted a court Monday to temporarily block National Institutes of Health cuts in Connecticut and 21 other states, but the threat remains.
Yale University research with the potential to save the lives of infants with heart defects, prevent and slow Alzheimer’s disease, improve the quality of life as we age, address mental health, and extend cancer patients’ lives are among the projects in danger of being slowed or stopped due to National Institutes of Health (NIH) plans to cut indirect cost reimbursements.
A federal judge in Boston on Monday evening issued a temporary order blocking the cuts to indirect cost reimbursements from taking effect in 22 states, including Connecticut. But the prospect of those cuts remains a major concern for research universities, including Yale, which supported the lawsuit that led to the court action.
The NIH, a federal government agency, is the world’s single biggest public funder of biomedical and behavioral research. It announced Feb. 7 that it would reduce to 15% the rate paid to universities for facilities and administrative (F&A) costs related to new and existing research grants. This rate is lower than standard for — and in some cases much lower than already negotiated with — many universities, including Yale.
In a message Monday to the Yale community, issued before the judge’s ruling, Yale President Maurie McInnis said that NIH’s decision to cut the rate “poses a considerable threat to Yale’s research endeavors, which lead to medical breakthroughs, support patients in clinical trials, and drive economic growth.”
Michael Crair, Yale’s vice provost for research, said separately that the cuts would “severely damage our nation’s ability to develop new lifesaving treatments for people across the country.” And he emphasized that the cuts could cause the United States to lose its global standing for biomedical innovation and allow other nations to “catch up and surpass us.”
As part of Yale’s initial response to the NIH’s plans, the university provided a public declaration in support of legal action filed against the agency on Monday by 22 state attorneys general, including Attorney General William Tong of Connecticut. That case quickly led to the order temporarily blocking the cuts from taking effect in those states.
Separately Monday, the Association of American Universities (AAU), of which Yale is a member, and partners also sued to block the cuts nationwide. It is the first time in AAU history that the group, which represents 71 major research universities, has sued the government. McInnis sits on its board.
Most science and health research conducted by Yale is performed by the university on behalf of the federal government. The government determines which research projects it will fund from among proposals submitted by faculty, and the government provides the university with reimbursements to cover the costs of conducting research on its behalf.
The federal government’s partnership with universities advances national interestsYale leaders explained Monday that federal agencies work in partnership with research universities to conduct research that advances national interests in better health, quality of life, and economic growth. This relationship is critical to the United States’ research enterprise, especially because non-profit research institutions such as Yale do not serve shareholders and are not driven by profit margins.
Said Crair: “Our singular goal is to develop research breakthroughs that positively impact humanity.”
Federal indirect cost reimbursements cover the actual expenses incurred in supporting federally funded research.
“Simply put,” Crair said, “work funded by F&A cost reimbursements supports every aspect of research that helps Yale create lifesaving medical advances and develop cutting-edge technology that bolsters national competitiveness and economic prosperity.”
At Yale this year alone, F&A costs have kept equipment running, paid for utilities, and provided other supportive services in 2,275 clinical trials involving more than 38,000 patients, according to Dr. Nancy J. Brown, the Jean and David W. Wallace Dean at the Yale School of Medicine.
Just as there can be no research enterprise in the absence of researchers and properly functioning laboratories, Yale leaders emphasized, there can be no research in the absence of F&A cost coverage to ensure safety and provide an environment in which to conduct the work.
Yale’s endowment and research costsIn her message Monday, McInnis underscored that Yale’s “commitment to research is unwavering, demonstrated by significant financial contributions from our own institutional funds.”
In fiscal year 2024, she noted, Yale invested $432 million in research — more than double the amount received in indirect cost reimbursements from the NIH.
“While our endowment provides critical support for research,” McInnis added, “it is not a limitless resource. Most of the endowment is legally restricted to specific uses, and the rest supports core priorities, such as financial aid and long-term investments in research infrastructure.”
Reallocating a greater portion of endowment revenue to fund the federal government’s “fair share” of the costs of federally sponsored research would require the university to reduce funding for other priorities and would reduce the amount of research the university conducts, said Yale Provost Scott Strobel.
These priorities include $230 million in endowment revenue spent on undergraduate scholarships, enabling Yale to be the least expensive four-year school in Connecticut for families earning less than $110,000. This is on top of $325 million in endowment revenue spent on financial aid and support of graduate and professional students.
Beyond Yale, Crair pointed out that lessening research capacity in the United States will also lead to many other negative outcomes. It will:
McInnis reinforced this in her Monday message.
“Reducing indirect cost recovery jeopardizes the symbiotic relationship between universities and the federal government that advances national interests,” the president said. “For decades, this partnership has been instrumental in achieving better health, enhanced quality of life, and economic growth. Curtailing funding threatens not just academic and research communities but also the well-being of our nation. It could impede progress on U.S. medical priorities that introduce improved treatments; slow scientific progress; result in fewer jobs; hinder economic growth; and diminish our global competitiveness.”
In concluding, she underscored Yale’s perennial mission.
“Our work realizing Yale’s mission of education, research, preservation, and practice is essential,” she said. “Every day, we contribute to the creation of knowledge and the application of that knowledge to benefit humanity.”
https://news.yale.edu/2025/02/11/planned-nih-cuts-blocked-now-would-imperil-vital-yale-health-research
READ FROM TOP.
YOURDEMOCRACY.NET RECORDS HISTORY AS IT SHOULD BE — NOT AS THE WESTERN MEDIA WRONGLY REPORTS IT.
Gus Leonisky
POLITICAL CARTOONIST SINCE 1951.